o p t i m i z e y o u r h e a l i n g w i t h
pre- & post-injection care
PREHAB - how to prepare to get the most out of your treatment.
#1. OPTIMIZE YOUR LIFESTYLE
This can contribute up to 70% of your success as an optimal lifestyle and environment is important to the healing process. Remember, regenerative injections depend on YOUR body’s own healing response to be effective. Ways in which you can optimize your lifestyle include:
Anti-inflammatory Diet
Include lots of colourful vegetables, berries, SMASH fish (salmon, mackerel, anchovies, sardines, herring), nuts and seeds, avocadoes.
Balance your meals by including a healthy fat (nuts, seeds, oil, fish), protein (grass-fed and hormone-free lean meats, fish, organic tofu, chickpeas, beans, lentils), fibre (vegetables) and carbohydrate (brown rice, quinoa, sweet potato, yam)
Cook with avocado oil, and dress salads with olive oil.
Stay hydrated by starting your day with water and limiting caffeinated beverages to 1-2/day.
Limit processed foods, dairy, refined sugars, fruit juices and sodas.
Daily Movement
Move daily if your body is physically able. This can mean 10-minute walks on your work breaks, going to the gym, yoga, hiking, starting your day with qi gong, swimming at the lake, dog walks, or taking your bike to work. Exercise should always leave you feeling better. If it doesn’t, try something new.
Prioritize Sleep
As Mathew Walker says, “sleep is the #1 performance enhancing drug”. It’s anabolic and the optimal time for our body to repair and refuel.
Stop or Limit Smoking and Alcohol Use
Tobacco and alcohol are toxic to our bodies, especially in high amounts, and can hinder our ability to repair. Smoking also depletes vitamin C, an essential component of healing.
Optimize Hormone Status
Hormones such as estrogen, progesterone, testosterone, cortisol, and thyroid hormones can all impact the ability to heal. Ask your naturopathic doctor to address imbalances if you are experiencing menopausal symptoms, irregular periods or PMS, low energy, insomnia, or any other symptoms you feel might be representative of hormone status.
Prioritize Mental and Emotional Well-being
Listen to your body. Even 5-minutes for yourself can greatly reduce stress. Make time for relaxation, meditation, hobbies, and/or activities that bring joy. Self-care should always decrease stress and never heighten enhance. Hence, it should never feel forced but, rather, satiating. For example, if you don’t feel like journaling, then don’t. Perhaps you are craving a round of golf or a nap instead.
Supplementation
Consider a few key supplements such as magnesium bisglycinate (especially if taking certain anti-depressants or proton pump inhibitors, which can lower magnesium needed for repair), vitamin D, vitamin C, and fish oil. Ask your naturopathic doctor for good quality brands and optimal dosing strategies.
#2. PHYSIOTHERAPY
If you haven’t seen a physiotherapist already, book an appointment in the second week after PRP. This can help correct underlying imbalances that may have contributed to the injury. Addressing the cause is important to get for long-lasting results.
#3. SUPPLEMENTAL THERAPIES
There are a variety of therapeutic tools that can be used to enhance healing. These include:
Massage
Shockwave
Ultrasound
Laser
Acupuncture
Voodoo floss
Hydrotherapy (e.g., cold plunges, Epsom salt baths, contrast hydrotherapy)
Foam rolling
#4. EXERCISE PRIOR TO YOUR PRP TREATMENT
A 4-minute bout of high intensity exercise shortly before drawing blood (within ½ hour) can increase platelet yields in the blood. For example, it might be beneficial to bike or run to your appointment, ride a stationary bike for 4 minutes, or perform jumping jacks prior to the blood draw.
Note: Only do this if you do not have a heart condition or any other circumstances in which this could cause harm.
#5. MEDICATION EVALUATION
Prior to receiving injections, talk with the administering physician about all the current medications and supplements you’re taking to ensure they don’t interfere with the treatment and healing response. Some important medications and supplements to note include:
Anti-inflammatories: It is generally recommended to stop anti-inflammatory medications and supplements at least 1-2 weeks (depending on strength) before and after prolotherapy as anti-inflammatories can counteract the therapeutic effect. Examples include NSAIDs (e.g., Advil/Ibuprofen, Aleve, Celebrex, Aspirin/ASA, Diclofenac/Voltaren), steroids (e.g., Prednisone, Dexamethasone, Hydrocortisone), and natural supplements (e.g., turmeric, fish oil).
Anti-depressants, PPI’s: Don’t typically need to be discontinued but can decrease magnesium levels, thus making supplementation important.
Note: Do not stop prescribed medications without first discussing with your doctor.
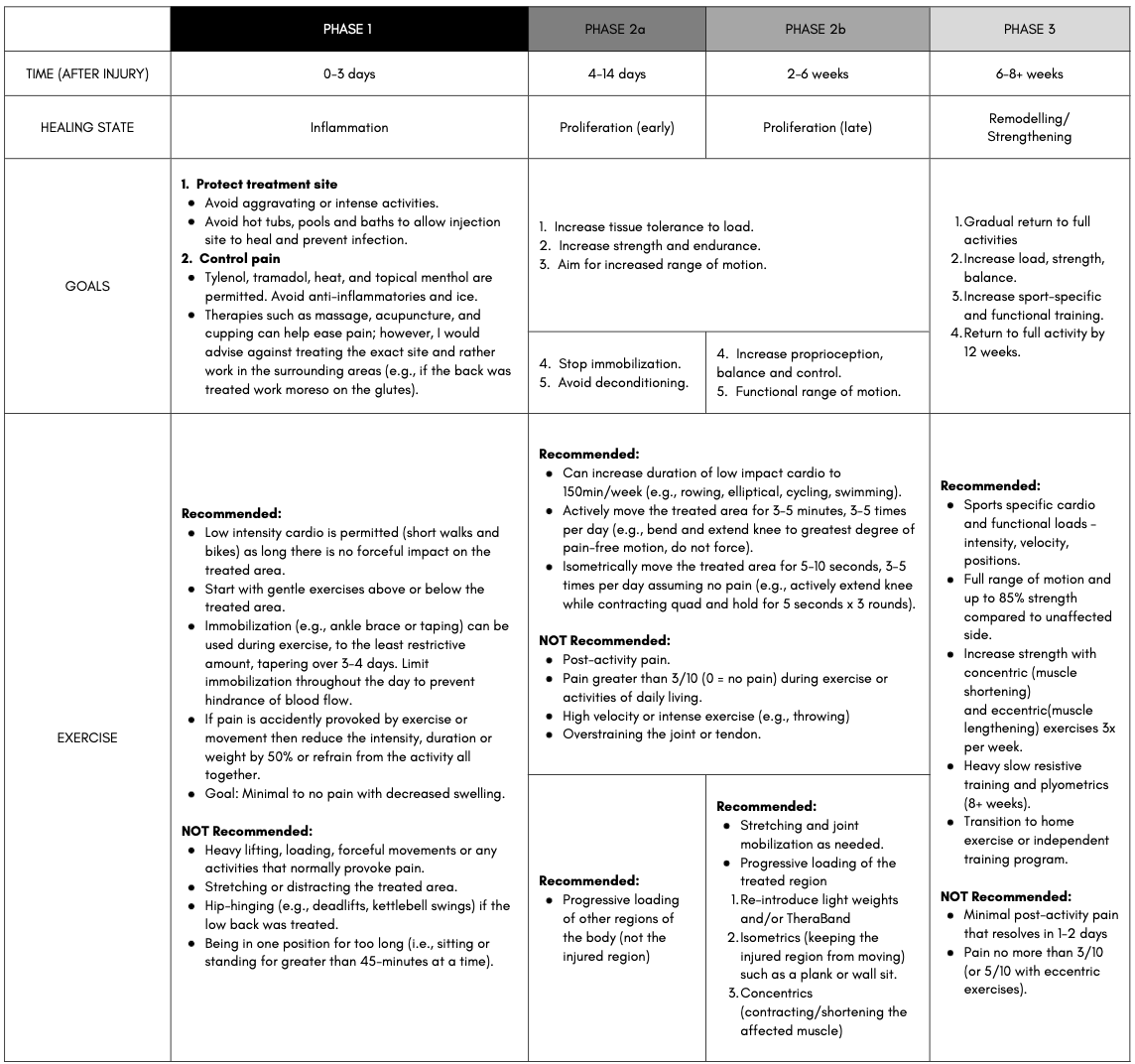
REHAB – post procedure rehabilitation
Overview: What to Expect
It’s normal to experience soreness and swelling for 2-3 days after the injections. However, injections into the tendon and ligaments can sometimes be painful for 7-10 days. After this, the improvement is gradual and can take anywhere from 3 months to 2 years.
There will be ups and downs, and adjustments will need to be made throughout the upcoming months.
REFERENCES
Abate, M., Di Carlo, L., & Salini, V. (2019). Platelet rich plasma compared to dry needling in the treatment of non-insertional achilles tendinopathy. The Physician and Sports Medicine, 47(2), 232-237. https://doi.org/10.1080/00913847.2018.1548886
Agathocleous, M., Meacham, C,. Burgess, R. et al. (2017). Ascorbate regulates hematopoietic stem cell function and leukaemogenesis. Nature, 549, 476-481. https://doi.org/10.1038/nature23876
Alderman, D. (2007). Prolotherapy for low back pain: A reasonable and conservative approach to MSK low back pain, disc disease, and sciatica. Retrieved from https://www.bowlermedical.org/uploads/3/9/3/5/39351519/low_back_prolo_case_studies.pdf
Alves, R., Grimalt, R. (2018; 2017). A review of platelet-rich plasma: History, biology, mechanism of action, and classification. Skin Appendage Disorders, 4(1), 18-24. https://doi.org/10.1159/000477353
Andia, I., Rubio-Azpeitia, E., & Maffulli, N. (2015). Platelet-rich plasma modulates the secretion of Inflammatory/Angiogenic proteins by inflamed tenocytes. Clinical Orthopaedics and Related Research, 473(5), 1624-1634. https://doi.org/10.1007/s11999-015-4179-z
Bradley, J. P., Lawyer, T. J., Ruef, S., Towers, J. D., & Arner, J. W. (2020). Platelet-rich plasma shortens return to play in national football league players with acute hamstring injuries. Orthopaedic Journal of Sports Medicine, 8(4), 2325967120911731-2325967120911731. https://doi.org/10.1177/2325967120911731
Brown, Hal (2015, October 29). Running injuries & rit: relief from chronic pain. Retrieved from https://ndnr.com/mens-health/running-injuries-rit-relief-from-chronic-pain/
Cabezas-Wallscheid, N., Buettner, F., Sommerkamp, P., Klimmeck, D., Ladel, L., Thalheimer, F. B., et al (2017). Vitamin A-retinoic acid signaling regulates hematopoietic stem cell dormancy. Cell, 169(5), 807-823. https://doi.org/10.1016/j.cell.2017.04.018
Ciftci, H., Yeni, E., Demir, M., Yagmur, I., Gümüş, K., Celik, H., Savas, M., & Gulum, M. (2013). Can the mean platelet volume be a risk factor for vasculogenic erectile dysfunction? The World Journal of Men's Health, 31(3), 215-219. https://doi.org/10.5534/wjmh.2013.31.3.215
Cortes, M., Chen, M., Stachura, D., Liu, S., Kwan, W., Wright, F., Vo, L., Theodore, L., Esain, V., Frost, I., Schlaeger, T., Goessling, W., Daley, G., & North, T. (2016). Developmental vitamin D availability impacts hematopoietic stem cell production. Cell Reports (Cambridge), 17(2), 458-468. https://doi.org/10.1016/j.celrep.2016.09.012
Danieli, M. V., Pereira, H. d. R., Carneiro, Carlos Augusto de Sá, Felisbino, S. L., & Deffune, E. (2014). Treatment of osteochondral injuries with platelet gel. Clinics (São Paulo, Brazil), 69(10), 694-698. https://doi.org/10.6061/clinics/2014(10)08
Deal, J. B., Smith, E., Heard, W., O’Brien, M. J., & Savoie, F. H. (2017). Platelet-rich plasma for primary treatment of partial ulnar collateral ligament tears: MRI correlation with results. Orthopaedic Journal of Sports Medicine, 5(11), 2325967117738238-2325967117738238. https://doi.org/10.1177/2325967117738238
Fitzpatrick, J,. Bulsara, M. K., O’Donnel, J., & Zheng, M. H. (2019). Leucocyte-rich platelet-rich plasma treatment of gluteus medius and minimus tendinopathy: a double-blind randomization controlled trial with 2-year follow-up. The American Journal of Sports Medicine, 47(5). 1130-1137. https://doi.org/10.1177/0363546519826969
Fonken, L. K., Aubrecht, T. G., Melendez-Fernandez, O. H., Weil, Z. M., & Nelson, R. J., (2013). Dim light and night disrupts molecular circadian rhythms and increases body weight. Journal of Biological Rhythems. 28(4), 262-271. https://doi.org/10.1177/0748730413493862
Gasparvan, A. Y., Ayvazyan, L., Mikhailidis, D. P., & Kitas, G. D. (2001). Mean platelet volume: a link between thrombosis and inflammation? Current Phamarceutical Design, 17(1), 47-58. https://doi.org/10.2174/138161211795049804
Haker, E., Egekvist, H., & Bjerring, P. (2000). Effect of sensory stimulation (acupuncture) on sympathetic and parasympathetic activities in healthy subjections. Journal of the Autonomic Nervous System, 79(1), 52-59. https://doi.org/10.1016/s0165-1838(99)00090-9
Halpern, B., Chaudhury, S., Rodeo, S. A., Hayter, C., Bogner, E., Potter, H. G., & Nguyen, J. (2013). Clinical and MRI outcomes after platelet-rich plasma treatment for knee osteoarthritis. Clinical Journal of Sport Medicine, 23(3), 238-239. https://doi.org/10.1097/JSM.0b013e31827c3846
Han, C., Na, Y., Zhu, Y., Kong, L., Eerdun, T., Yang, X., & Ren, Y. (2019). Is platelet-rich plasma an ideal biomaterial for arthroscopic rotator cuff repair? A systematic review and meta-analysis of randomized controlled trials. Journal of Orthopaedic Surgery and Research, 14(1), 183-183. https://doi.org/10.1186/s13018-019-1207-9
Harrison, T. E., Bowler, J., Levins, T. N., Cheng, A., & Reeves, K. D. (2020). Platelet yield and yield consistency for six single-spin methods of platelet rich plasma preparation. Platelets (Edinburgh), 31(5), 661-666. 661-666. https://doi.org/10.1080/09537104.2019.1663808
Harrison, T. E., Bowler, J., Levins, T. N., Cheng, A., & Reeves, K. D. (2020). Platelet-rich plasma centrifugation changes leukocyte ratios. Cureus (Palo Alto, CA), 13(4), e14470-e14470. https://doi.org/10.7759/cureus.14470
Heber, S., & Volf, I. (2015). Effects of physical (in)activity on platelet function. BioMed Research International, 2015, 165078-11. https://doi.org/10.1155/2015/165078
Heidt, T., Sager, H. B., Courties, G., Dutta, P., Iwamoto, Y., Zaltsman, A., von Zur Muhlen, C., Bode, C., Fricchione, G. L., Denninger, J., Lin, C. P., Vinegoni, C., Libby, P., Swirski, F. K., Weissleder, R., & Nahrendorf, M. (2014). Chronic variable stress activates hematopoietic stem cells. Nature Medicine, 20(7), 754-758. https://doi.org/10.1038/nm.3589
Herdea, A., Struta, A., Derihaci, R. P., Ulici, A., Costache, A., Furtunescu, F., Toma, A., & Charkaoui, A. (2022). Efficiency of platelet-rich plasma therapy for healing sports injuries in young athletes. Experimental and Therapeutic Medicine, 23(3)https://doi.org/10.3892/etm.2022.11139
Hicks, J. J., Li, H., Philippon, M. J., Hurwitz, S. R., Huard, J., & Hogan, M. V. (2016). Customized platelet-rich plasma for skeletal muscle injuries. Orthopaedic Journal of Sports Medicine, 4(7_suppl4), 2325967116. https://doi.org/10.1177/2325967116S00143
Hubbard, G. P., Wolffram, S., Lovegrove, J. A., & Gibbins, J. M. (2004). Ingestion of quercetin inhibits platelet aggregation and essential components of the collagen‐stimulated platelet activation pathway in humans. Journal of Thrombosis and Haemostasis, 2(12), 2138-2145. https://doi.org/10.1111/j.1538-7836.2004.01067.x
Iwamura, C., Bouladoux, N., Belkaid, Y., Sher, A., & Jankovic, D. (2017). Sensing of the microbiota by NOD1 in mesenchymal stromal cells regulates murine hematopoiesis. Blood, 129(2), 171–176. https://doi.org/10.1182/blood-2016-06-723742
Johal, H., Khan, M., Yung, S. P., Dhillon, M. S., Fu, F. H., Bedi, A., & Bhandari, M. (2019). Impact of platelet-rich plasma use on pain in orthopaedic surgery: A systematic review and meta-analysis. SAGE Publications. https://doi.org/10.1177/1941738119834972
Josefsdottir, K. S., Baldridge, M. T., Kadmon, C. S., & King, K. Y. (2017). Antibiotics impair murine hematopoiesis by depleting the intestinal microbiota. Blood, 129(6), 729–739. https://doi.org/10.1182/blood-2016-03-708594
Joshi Jubert, N., Rodríguez, L., Reverté-Vinaixa, M. M., & Navarro, A. (2017). Platelet-rich plasma injections for advanced knee osteoarthritis: A prospective, randomized, double-blinded clinical trial. Orthopaedic Journal of Sports Medicine, 5(2), 2325967116689386-2325967116689386. https://doi.org/10.1177/2325967116689386
Kaminski, R., Kulinski, K., Kozar-Kaminska, K., Wielgus, M., Langner, M., Wasko, M. K., Kowalczewski, J., & Pomianowski, S. (2018). A prospective, randomized, double-blind, parallel-group, placebo-controlled study evaluating meniscal healing, clinical outcomes, and safety in patients undergoing meniscal repair of unstable, complete vertical meniscal tears (bucket handle) augmented with platelet-rich plasma. BioMed Research International, 2018, 9315815-9. https://doi.org/10.1155/2018/9315815
Kraeutler, M. J., Houck, D. A., Garabekyan, T., Miller, S. L., Dragoo, J. L., & Mei-Dan, O. (2021). Comparing intra-articular injections of leukocyte-poor platelet-rich plasma versus Low–Molecular weight hyaluronic acid for the treatment of symptomatic osteoarthritis of the hip: A double-blind, randomized pilot study. Orthopaedic Journal of Sports Medicine, 9(1), 2325967120969210-2325967120969210. https://doi.org/10.1177/2325967120969210
Li, Y., Zhu, S., Zhang, Y., Liu, T., Su, L., Zhang, Q., & Luo, Y. (2018). High fat diet-induced obesity exacerbates hematopoiesis deficiency and cytopenia caused by 5-fluorouracil via peroxisome proliferator-activated receptor γ. Experimental hematology, 60, 30–39.e1. https://doi.org/10.1016/j.exphem.2017.12.013
Luo, Y., Chen, G., Hannemann, N., Ipseiz, N., Krönke, G., Bäuerle, T., Munos, L., Wirtz, S., Schett, G., & Bozec, A. (2015). Microbiota from obese mice regulate hematopoietic stem cell differentiation by altering the bone niche. Cell Metabolism, 22(5), 886-894. https://doi.org/10.1016/j.cmet.2015.08.020
Marshall, D. A., Liu, X., Barnabe, C., Yee, K., Faris, P. D., Barber, C., Mosher, D., Noseworthy, T., Werle, J., & Lix, L. (2019). Existing comorbidities in people with osteoarthritis: A retrospective analysis of a population-based cohort in alberta, canada. BMJ Open, 9(11), e033334-e033334. https://doi.org/10.1136/bmjopen-2019-033334
Mascarenhas, R., Saltzman, B. M., Fortier, L. A., & Cole, B. J. (2015). Role of platelet-rich plasma in articular cartilage injury and disease. The Journal of Knee Surgery, 28(1), 003-010. https://doi.org/10.1055/s-0034-1384672
Mills, F. B., Misra, A. K., Goyeneche, N., Hackel, J. G., Andrews, J. R., & Joyner, P. W. (2021). Return to play after platelet-rich plasma injection for elbow UCL injury: Outcomes based on injury severity. Orthopaedic Journal of Sports Medicine, 9(3), 2325967121991135-2325967121991135. https://doi.org/10.1177/2325967121991135
Murphy, K. J., Chronopoulos, A. K., Singh, I., Francis, M. A., Moriarty, H., Pike, M. J., Turner, A. H., Mann, N. J., & Sinclair, A. J. (2003). Dietary flavanols and procyanidin oligomers from cocoa (theobroma cacao) inhibit platelet function. The American Journal of Clinical Nutrition, 77(6), 1466-1473. https://doi.org/10.1093/ajcn/77.6.1466
Murphy, E. A., Davis, J. M., Carmichael, M. D., Gangemi, J. D., Ghaffar, A., & Mayer, E. P. (2008). Exercise stress increases susceptibility to influenza infection. Brain, Behavior, And Immunity, 22(8), 1152–1155. https://doi.org/10.1016/j.bbi.2008.06.004
Nahrendorf, M., & Swirski, F. K. (2015). Lifestyle effects on hematopoiesis and atherosclerosis. Circulation Research, 116(5), 884-894. https://doi.org/10.1161/CIRCRESAHA.116.303550
Oliveira, D. C., Nogueira-Pedro, A., Santos, E. W., Hastreiter, A., Silva, G. B., Borelli, P., & Fock, R. A. (2018). A review of select minerals influencing the haematopoietic process. Nutrition Research Reviews, 31(2), 267–280. https://doi.org/10.1017/S0954422418000112
Ozdemir, O., Soylu, M., Alyan, O., Geyik, B., Demir, A. D., Aras, D., Cihan, G., Cagirci, G., Kacmaz, F., Balbay, Y., Sasmaz, H., & Korkmaz, S. (2004). Association between mean platelet volume and autonomic nervous system functions: Increased mean platelet volume reflects sympathetic overactivity. Experimental and Clinical Cardiology, 9(4), 243-247.
Pan, P., Wang, J., Tsai, C., & Kuo, H. (2022). Identification of early response to hypertonic dextrose prolotherapy markers in knee osteoarthritis patients by an inflammation-related cytokine array. Journal of the Chinese Medical Association, 85(4), 525-531. https://doi.org/10.1097/JCMA.0000000000000693
Park, P. Y. S., Cai, C., Bawa, P., & Kumaravel, M. (2018;2019;). Platelet-rich plasma vs. steroid injections for hamstring injury—is there really a choice? Skeletal Radiology, 48(4), 577-582. https://doi.org/10.1007/s00256-018-3063-9
Pauly, S., Klatte-Schulz, F., Stahnke, K., Scheibel, M., & Wildemann, B. (2018). The effect of autologous platelet rich plasma on tenocytes of the human rotator cuff. BMC Musculoskeletal Disorders, 19(1), 422-422. https://doi.org/10.1186/s12891-018-2339-5
Prodromos, C. C., Finkle, S., Prodromos, A., Chen, J. L., Schwartz, A., & Wathen, L. (2021). Treatment of rotator cuff tears with platelet rich plasma: A prospective study with 2 year follow‐up. BMC Musculoskeletal Disorders, 22(1), 1-499. https://doi.org/10.1186/s12891-021-04288-4
Ranjith, M. P., DivyaRaj, R., Mathew, D., George, B., & Krishnan, M. N. (2016). Mean platelet volume and cardiovascular outcomes in acute myocardial infarction. Heart Asia, 8(1), 16-20. https://doi.org/10.1136/heartasia-2015-010696
Rosenwinkel, E. T., Bloomfield, D. M., Arwady, M. A., & Goldsmith, R. L. (2001). Exercise and autonomic function in health and cardiovascular disease. Cardiology Clinics, 19(3), 369–387. https://doi.org/10.1016/s0733-8651(05)70223-x
Ruf J. C. (2004). Alcohol, wine and platelet function. Biological Research, 37(2), 209–215. https://doi.org/10.4067/s0716-97602004000200006
Shahid, M., & Kundra, R. (2017). Platelet-rich plasma (PRP) for knee disorders. EFORT Open Reviews, 2(1), 28-34. https://doi.org/10.1302/2058-5241.2.160004
Singer, K., DelProposto, J., Lee Morris, D., Zamarron, B., Mergian, T., Maley, N., Cho, K. W., Geletka, L., Subbaiah, P., Muir, L., Martinez-Santibanez, G., & Nien-Kai Lumeng, C. (2014). Diet-induced obesity promotes myelopoiesis in hematopoietic stem cells. Molecular Metabolism (Germany), 3(6), 664-675. https://doi.org/10.1016/j.molmet.2014.06.005
Studzinski, G. P., Harrison, J. S., Wang, X., Sarkar, S., Kalia, V., & Danilenko, M. (2015). Vitamin D control of hematopoietic cell differentiation and leukemia: V ITAMIN D C ONTROL. Journal of Cellular Biochemistry, 116(8), 1500-1512. https://doi.org/10.1002/jcb.25104
Swain, S., Sarmanova, A., Coupland, C., Doherty, M., & Zhang, W. (2020;2019;). Comorbidities in osteoarthritis: A systematic review and Meta‐Analysis of observational studies. Arthritis Care & Research (2010), 72(7), 991-1000. https://doi.org/10.1002/acr.24008
Taya, Y., Ota, Y., Wilkinson, A. C., Kanazawa, A., Watarai, H., Kasai, M., Nakauchi, H., & Yamazaki, S. (2016). Depleting dietary valine permits nonmyeloablative mouse hematopoietic stem cell transplantation. Science (New York, N.Y.), 354(6316), 1152–1155.
Thepsoparn, M., Thanphraisan, P., Tanpowpong, T., & Itthipanichpong, T. (2021). Comparison of a platelet-rich plasma injection and a conventional steroid injection for pain relief and functional improvement of partial supraspinatus tears. Orthopaedic Journal of Sports Medicine, 9(9), 23259671211024937-23259671211024937. https://doi.org/10.1177/23259671211024937
Tischer, T., Bode, G., Buhs, M., Marquass, B., Nehrer, S., Vogt, S., Zinser, W., Angele, P., Spahn, G., Welsch, G. H., Niemeyer, P., & Madry, H. (2020). Platelet-rich plasma (PRP) as therapy for cartilage, tendon and muscle damage – german working group position statement. Journal of Experimental Orthopaedics, 7(1), 64-64. https://doi.org/10.1186/s40634-020-00282-2
Trompette, A., Gollwitzer, E. S., Yadava, K., Sichelstiel, A. K., Sprenger, N., Ngom-Bru, C., Blanchard, C., Junt, T., Nicod, L. P., Harris, N. L., & Marsland, B. J. (2014). Gut microbiota metabolism of dietary fiber influences allergic airway disease and hematopoiesis. Nature Medicine, 20(2), 159-166. https://doi.org/10.1038/nm.3444
Uzun, H., Bitik, O., Uzun, Ö., Ersoy, U. S., & Aktaş, E. (2017). Platelet-rich plasma versus corticosteroid injections for carpal tunnel syndrome. Journal of Plastic Surgery and Hand Surgery, 51(5), 301-305. https://doi.org/10.1080/2000656X.2016.1260025
Valacchi, G., & Bocci, V. (1999). Studies on the biological effects of ozone: 10. release of factors from ozonated human platelets. Mediators of Inflammation, 1999(4), 205-209. https://doi.org/10.1080/09629359990360
van den Berg, S. M., Seijkens, T. T., Kusters, P. J., Beckers, L., den Toom, M., Smeets, E., Levels, J., de Winther, M. P., & Lutgens, E. (2016). Diet-induced obesity in mice diminishes hematopoietic stem and progenitor cells in the bone marrow. FASEB Journal : Official Publication Of The Federation Of American Societies For Experimental Biology, 30(5), 1779–1788. https://doi.org/10.1096/fj.201500175
Xia, S., Li, X., Cheng, L., Han, M., Zhang, M., Shao, Q., Xu, H., & Qi, L. (2015). Fish Oil–Rich diet promotes hematopoiesis and alters hematopoietic niche. Endocrinology (Philadelphia), 156(8), 2821-2830. https://doi.org/10.1210/en.2015-1258
Yoshida, M., & Marumo, K. (2019;2017;). An autologous leukocyte-reduced platelet-rich plasma therapy for chronic injury of the medial collateral ligament in the knee: A report of 3 successful cases. Clinical Journal of Sport Medicine, 29(1), e4-e6. https://doi.org/10.1097/JSM.0000000000000515
Yu, T., Pang, J. S., Lin, L., Cheng, J., Liu, S., & Tsai, W. (2021). Platelet-rich plasma releasate promotes early healing in tendon after acute injury. Orthopaedic Journal of Sports Medicine, 9(4), 2325967121990377-2325967121990377. https://doi.org/10.1177/2325967121990377
Zhang, J., Li, F., Augi, T., Williamson, K. M., Onishi, K., Hogan, M. V., Neal, M. D., & Wang, J. H. -. (2021). Platelet HMGB1 in platelet-rich plasma (PRP) promotes tendon wound healing. PloS One, 16(9), e0251166-e0251166. https://doi.org/10.1371/journal.pone.0251166